Pour some milk in a bottle and give it to your baby… sounds simple enough, right?
As a pregnant soon-to-be mom doing my research, I realized quickly that I actually didn’t know the first thing about bottle feeding.
This post will cover 6 important things worth learning about bottle feeding breastmilk and/or formula.
There may be affiliate links in this post. Read this disclosure policy to learn more.

Efficiently warming a bottle.
Whether you’re bottle feeding formula or breastmilk, if it’s been in the fridge, you’re probably going to want to warm it before giving it to baby.
If your baby will take it cold, consider yourself lucky! Aden never needed his bottles to actually be warm, just room temperature.
It was news to me as a first time mom that you can’t just stick a bottle in the microwave. Milk can heat unevenly, creating hot spots that will burn a baby’s mouth.

Your options are to:
- Run the bottle under hot water (least efficient option)
- Microwave water in a mug/bowl and place the bottle in the hot water (our fave)
- Buy a bottle warmer
We decided against purchasing a bottle warmer because the heating time was no faster than microwaving a cup of water for a minute and placing the bottle in the cup to warm for a couple of minutes.
No matter which bottle heating method you choose, be sure to test the temperature before feeding by squirting a few drops onto your wrist.

Mixing temperatures is a no-no.
Here’s another best practice I didn’t know about bottle feeding…
Let’s say you’ve got some breastmilk sitting in the refrigerator from an earlier pump session. Then later, you pump again and you want to add the new milk to the refrigerated stash.
Guess what… you shouldn’t just combine them without a little prep work.
Milk should be combined at the same temperature to discourage bacterial growth. This means not mixing fresh with room temperature milk, or mixing fresh with refrigerated milk.
It’s perfectly fine to combine milk from separate pumping sessions, but it’s best to bring the liquids to the same temperature before you mix them.
The easiest thing to do is just refrigerate the fresh milk in a separate container and then combine everything later once it’s all cold.
This milk storage best practice comes from food safety guidelines. Bacteria grows rapidly between 40 and 140 degrees Fahrenheit, the “danger zone.”
I was never a huge pumper so I just bought a few extra collection bottles for my Spectra. I put them in the fridge and then combined as needed.


Milk spoils so freaking quickly!
As a new mom, I was blown away by how strict the guidelines are for discarding breastmilk and formula!
This is really important for all bottle-feeding parents to know…
Each category has its own rules put forth by the AAP and the CDC. I’ll cover 3 of them here:
★ Bottle of formula baby drank from: If baby starts, but doesn’t finish a bottle, you have only ↠ 1 hour ↞ to use the formula. Whatever’s left in the bottle needs to be ditched at that point. What surprised me was that you can’t just refrigerate the remaining milk. Bacteria from baby’s mouth can still multiply in the refrigerator.
★ Open container of formula: Let’s say you buy a big container of ready-to-feed formula. You break the seal to pour some into a bottle. From that point on, you have ↠ 48 hours ↞ to finish the container. Whatever’s left must be discarded.
★ Bottle of breast milk baby drank from: You’ve got a bit more leeway with breast milk than formula. If baby starts, but doesn’t finish a bottle, you have ↠ 2 hours ↞ to use the breast milk before ditching it.
There are lots of other guidelines for proper storage and preparation of breast milk that you should read on the CDC’s website.

Buying a sterilizer is totally unnecessary.
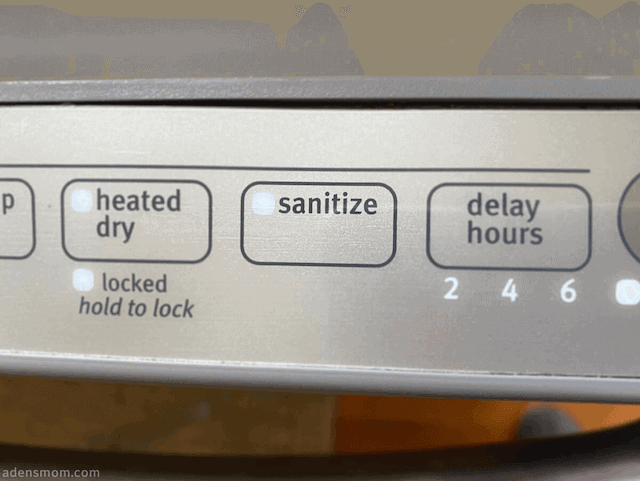
The best way to sterilize bottles and pump parts is to boil them in water or use your dishwasher’s Sanitize setting.
We initially bought a sterilizer, thinking it would make it easier to clean the bottles each day… however we returned it as soon as we read in the manual that you still have to wash the bottles before sterilizing them each time. Super inefficient!
That said, don’t get a sterilizer. Save that precious spot on your baby registry for something you’ll actually use.

If you’re a first time parent and are new to all of this as I was, here’s what you need to know about sterilizing:
- You should sterilize all bottles, pump parts, pacifiers, and feeding supplies before first use.
- You will probably also want to sterilize them daily when your baby is young.
The CDC advises:
“Sanitizing is particularly important when your baby is younger than 3 months, was born prematurely, or has a weakened immune system.”
There is more than one effective way to sterilize, but we chose to have one method for “before first use” and another daily method.
Before first use: Boil water in a big pot. Boil hard plastic parts for 5 minutes. If the parts are soft rubber (silicone), boil for 2 minutes.
Daily sterilizing: We sterilized bottles and pump parts daily during Aden’s first 3 months by using our dishwasher’s Sanitize setting.

There are different stages of nipples.
As a first time mom, I had absolutely no idea why my newborn seemed to cough and gag on some bottles and not others.
It wasn’t until months later that I realized I had bought the same Tommee Tippee bottles but with different nipple stages.
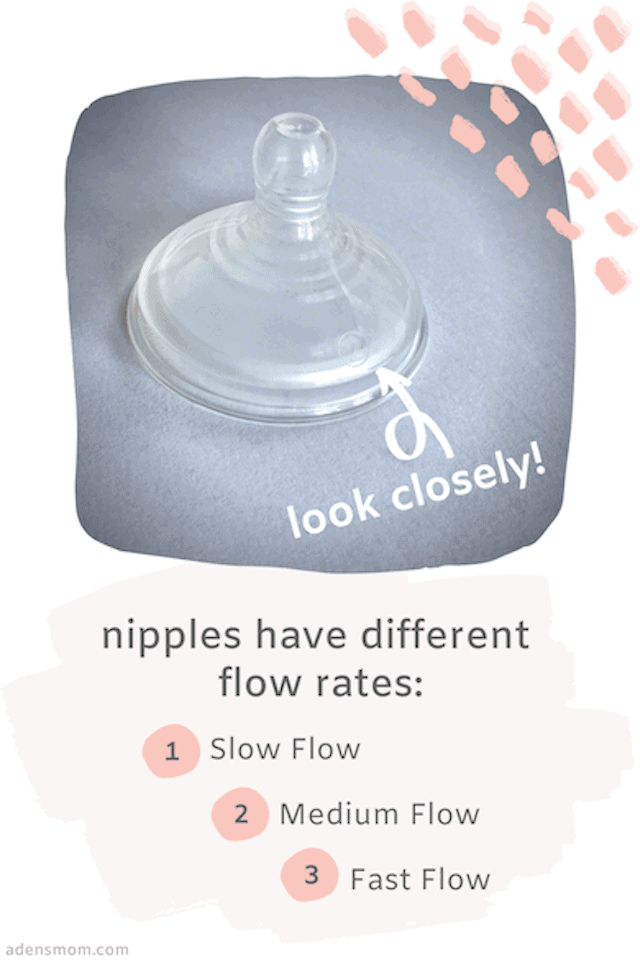
Most brands’ nipples have a “flow rate” graduation similar to this: (1) Slow flow; (2) Medium flow; (3) Fast flow.
Tommee Tippee also makes an extra slow flow nipple — which I later realized was best for Aden’s first weeks!
If you want to double check the stage you bought, you can tell by looking closely at the nipple for a raised number that corresponds to the flow stage.
Newborns need extra slow or slow flow nipples. Depending on whether you’re breastfeeding, you might want to move up to the next level when your baby turns 3 months and 6 months, respectively. Avent has a good guide if you want to learn more.


Bottles and nipples should be discarded every few months.
This is important: You should read the packaging that comes with your bottles to see if there is a suggested lifespan for the bottle and/or nipple.
Since I used Tommee Tippee in the previous example, I will share their guidelines here:
“For safety and hygiene reasons it’s recommended that the feeding nipple is replaced every 2-months or sooner if damage or weakness is noticed.”
Tommee Tippee does not provide a lifespan for the bottles themselves.
Note: I’ve often seen it recommended to replace the bottles themselves every 6-months (not just the nipples). If you want to err on the side of caution, this isn’t a bad idea. However, I have yet to locate any evidence-based information about this. Each manufactuerer might have different recommendations, so again, be sure to read the insert or packaging that comes with your bottles.
Beware, so much of what you read on the internet about bottle feeding is bullshit.
You’ll notice that above I have linked to my sources, the AAP and the CDC.
There are endless websites filled with unscientific, unsubstantiated information. I was shocked to see how popular and “well-established” some of these appear.
Two of the worst offenders are KellyMom and La Leche League. Do not put your baby’s safety (or your own mental health) in the hands of these sites.
If you’re reading about bottle feeding and start seeing words like “nipple confusion” or “paced feeding,” your radar should go off that you’ve likely left the land of scientific evidence.
–
Hopefully, this has been a good start to your bottle feeding education. If you have questions about any of this, I encourage you to check out the links in the post.
I want to thank this evidence-based Facebook group for introducing me to many of these AAP and CDC guidelines.
Want more advice on getting ready for baby? Check out 35 Things to do Before Baby (while lying in bed!)

 Follow on Pinterest
Follow on Pinterest